Introduction
Scand J Plast Reconstr Surg Hand Surg 2003; 37: 332-338
S. M. BalajiBalaji Dental and Craniofacial Hospital, Teynampet, Chennai, India
Abstract.
Correction of one of the abnormal features is never enough to alleviate the entire deformity in a patient with a unilateral cleft lip and deformed nose, because the factors that led to the nasal deformity have already produced changes in the lower lateral cartilage, nostril, columella, septum, and alar base. These changes should be treated together with the contributory factors. By restoring the balance of the muscles by primary repair of the lip, orthodontic treatment, and orthognathic surgery, a more symmetric skeletal base can be established. The method of repair of the lip will also influence the deformity. Bone grafting can augment the skeletal base, but it will not improve the position of the lower lateral cartilage or the deviated septum. In this paper we describe a single stage correction of all the irregularities of the nose in patients with unilateral clefts which alleviates the asymmetrical nasal deformity.
Key words: unilateral cleft, septal deviation, alar base repositioning, tip projection, columella straightening.
Correspondence to: S. M. Balaji, MDS, Balaji Dental and Craniofacial Hospital, 30/1, KB. Dasan Road, Teynampet, Chennai 600 018, India. (Fax: 91-44-432 2907. E-mail: [email protected])
Accepted 31 October 2002
The nasal deformity in both complete and incomplete unilateral clefts is complex, and it can be corrected most successfully when it is symmetrical. Correction of the nasal deformity in unilateral cleft lip presents a difficult problem (4, 9) because it is asymmetrical. For many years the focus was on repair of the lip and palate rather than on correction of the nasal deformity. After closure of the lip, the deformity of the nasal tip and the nostrils preserved the stigma of the patient with a cleft lip and palate (CLP). Only recently have attempts been made to correct this deformity at the time of primary repair of the lip. Examination of the long-term results of primary rhinoplasty, reported by McComb (12) and McComb and Coghlan (13), suggested that there is no decrease in the overall size of the nose after primary nasal correction, but the shape is not entirely normal either. It is possible that the scar produced on one side of the cartilage where the perichondrium was exposed causes the growing cartilage to warp slightly on that side, so secondary repair of the deformity is required even after primary correction.
The nasal deformity in unilateral cleft
The first and most complete description of the nasal deformity associated with the unilateral cleft was published by Huffman and Lierle (10). The deformity affects the columella, nasal tip, ala, and lower lateral cartilages. In unilateral clefts the initial nasal deformity may differ from that which develops subsequent to primary repair of the cleft lip. The complex nasal deformity in these patients is partly the result of the anomaly itself and partly a result of previous corrective surgery. Recently, Cutting et al. (5) studied deformities in skin envelopes that resulted from rotation-advancement repair (Millard’s technique (5, 14)), and triangular flap repair (Bardach‘s modified technique (5)) of a cleft lip. Neither group had primary nasal correction. There were significant differences between the skin envelopes in the horizontal dimension in the two groups. In the rotation-advancement group the position of the alar base was considerably more normal, whereas in the triangular flap repair group the alar base was more lateral. On the other hand, the rotation- advancement group had a more pronounced deficiency in the horizontal alar base than the triangular flap repair group. This deficiency usually resulted in a small nostril in the rotation-advancement group.
According to Geoffrey and Hallock (6), Tennison’s technique of lip repair, which was modified by Trevaskis et al. (25) resulted in severe buckling of the alar rim. There are deficiencies in the region of the cleft in both the soft tissue and the facial skeleton.
One of the most important defects that requires correction in the secondary cleft lip nasal deformity is the lack of skeletal support beneath the alar base, which is often quite severe. The foot of the medial crus is positioned posteriorly on the cleft side relative to the other side. There is hypoplasia of the skeletal base in both complete and partial clefts, and that of the lesser maxillary segment is most common along its edges and at the edge of the piriform aperture (2). Milder deformities may be corrected successfully during the primary repair of the cleft lip using the techniques described by Millard and Morovic (14), McComb (12, 13), Salyer (2l,22) or Mulliken and Martinez-Perez (16).
The columella and nasal septum may also be affected by the morphological changes associated with the unilateral cleft. Because the medial crus of the lower lateral cartilage is shorter on the cleft side, the columella is also shorter, and it is pulled to the non-cleft side by the muscles that enter its base and join the orbicularis oris muscle. The degree and severity of the deformities vary greatly, and not all are present in every patient. According to LaRossa and Donnath (11), Gubisch et al. (7) Gubisch (8, 9) and Cutting et al. (5), the deformities include a short and slanted columella with its base deviated to the non-cleft side; a lateral crus of the lower lateral cartilage buckled into an S or M-shaped fold; a lateral crus of the lower lateral cartilage longer on the cleft side; the lower lateral
cartilage and nasal tip displaced backwards and downwards; an asymmetrical nasal tip with flattened ala resulting in a broad nose; a smaller (rotation flap) or larger (triangular flap) external nares than that on the non-cleft side; the base of the ala displaced laterally, posteriorly or inferiorly; a lowered nasal floor on the cleft side; a nasolabial fistula; deflection of the lower edge of the nasal septum and the anterior nasal spine into the non-cleft side; a deviated nasal septum; a hypertrophic lower turbinate on the cleft side; an asymmetrical nasal pyramid; a hypoplastic maxilla on the cleft side; and repositioning of the entire nostril.
Numerous methods have been described for the correction of this gross deformity, but single satisfactory method has given satisfactory results to set the standard for rhinoplasty in patients with unilateral CLP. Total correction of such deformity is a challenge. The external approach (open rhinoplasty under direct vision) gives better results even though scarring cannot be avoided. A combination of procedures is essential to give a stable and satisfactory result.
The procedures that have been combined are augmentation of the tip and bridge using grafts; septoplasty; V-Y plasty of the alar base; piriform augmentation; lateral crural augmentation; reduction of the ala; straightening of the columella; turbinoplasty; lateral osteotomy; alveolar bone grafting and philtral repair. The challenges are scars from the primary repair, management of the soft tissues, to shape the memory of the alar cartilages, intraoperative swelling that can obscure the surgeon’s perception of the shape of the nose and shrinking of the grafted cartilage.
The purpose of this paper is to present our current approach and selection of techniques in the correction of the nasal deformity associated with severe unilateral cleft lip.
PATIENTS AND METHOD
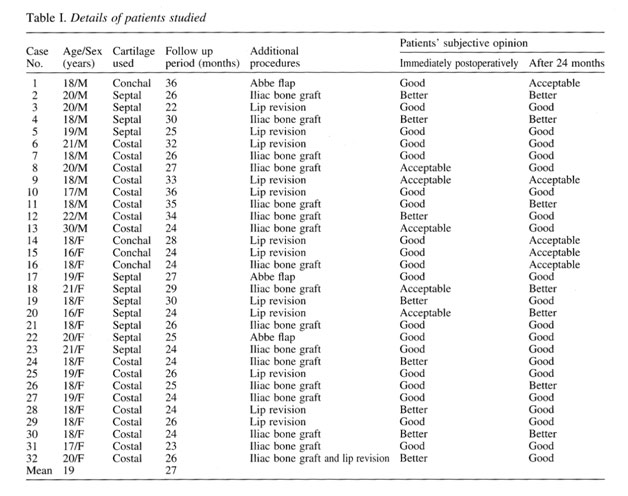
A total of 32 patients with severe unilateral cleft lip and nasal deformities were operated on from March 1998 to October 1999. These were 19 women and 13 men, mean age 19 years (range 16 to 30). Conchal cartilage was harvested in four patients, septal cartilage in 11, and costal cartilage in 17. Onlay iliac or costal synchondrosis grafts were used for the depressed piriform fossa in 17 cases. The patients were regularly monitored for a mean period of 27 months (range 23-36). The patients were asked to rate their appearance as good, better than before, acceptable, or worse than before after suture removal and 24 months later (Table I).
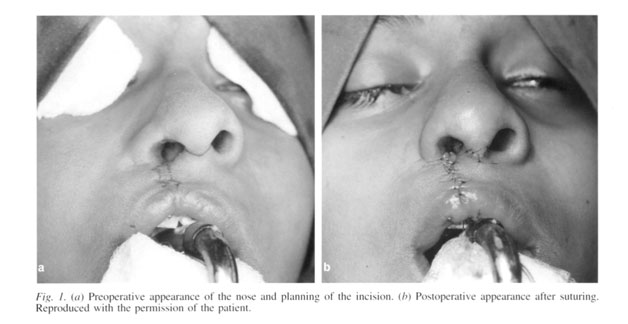
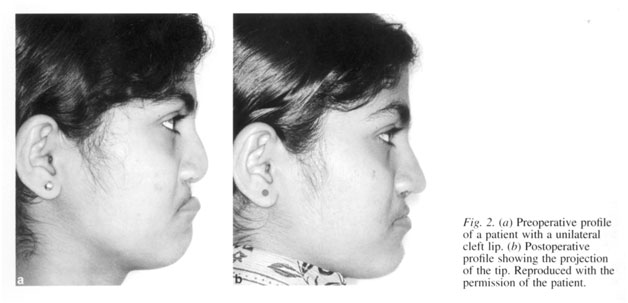
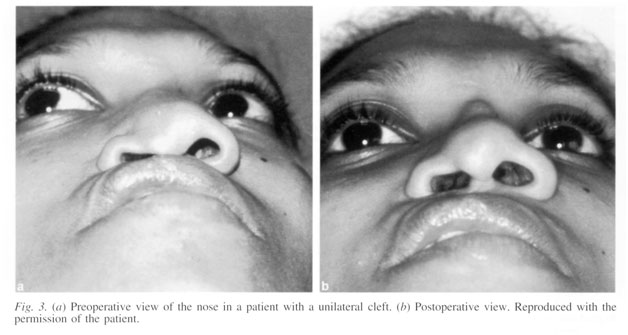
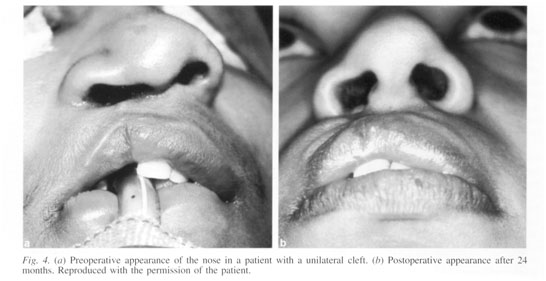
Surgical technique (Figs. 1-4)
All operations were done under general anaesthesia with oral intubation. A transcolumellar incision was made on the thinnest portion of the columella and combined with a reverse U incision and V-Y plasty. In some cases the lip scar was included, when the scar needed to be revised and the alar base required advancement. By using blunt and sharp dissection, both lower and upper lateral cartilages were fully exposed as far as the lower part of the nasal bones. Any loose fatty connective tissue was stripped away. At the septal angle the mucoperichondrial membrane was raised and detached from the upper lateral cartilage as far as the anterior nasal spine, maxillary crest, and vomerine plate. If the septal deviation was only mild, the convex surface was scored to make it even.
Moderate or severe deviation was corrected by excision of at least 10 mm of the anterosuperior margin of the most deviated part of the septal cartilage. The remaining septal cartilage was scored. The dislocated portion of the septal cartilage was fixed into the anterior nasal spine as a “strut graft” to straighten the columella and project the tip. The asymmetrical hump on the nasal bridge was removed with an osteotome.
The lateral osteotomy was made through a nasal mucosal approach at the piriform aperture. Both the upper lateral cartilages near the lower portion of the nasal bone were approximated to maintain the stability of the fractured nasal bone and to support the nasal pyramid after the osteotomy. The lower and upper lateral cartilage on the cleft side were mobilised as far as the non-cleft lower lateral cartilage.
The asymmetrical lower lateral cartilage was sculpted to resemble the normal side. When the lower lateral cartilage was thin, rudimentary, or had been spoilt by previous surgery, a conchal or septal cartilage was shaped and used as an onlay graft to create a dome, as described by Sheen (23).
If there was still insufficient projection of the nasal tip after the repositioning and shaping of the lower lateral cartilage on the cleft side, additional cartilage was harvested from the septum or the concha and was used as a shield graft to augment the nasal tip. In some cases, Peck et al.’s (19) umbrella graft was used instead of an individual strut and shield graft.
When the columella was extremely stunted and the nasal spine rudimentary, a costal graft was harvested through an inframammary incision, fixed to an “L” plate, and screwed to the maxilla at the base of the nasal spine to lengthen and straighten the columella. In some cases when the height of the nasal septum was reduced, a longer piece of costal cartilage was harvested to augment the dorsum of the nose and inserted beneath the perichondrium and above the nasal pyramid.
When a depressed piriform aperture was combined with an alveolar cleft, a corticocancellous graft was harvested from the anterior iliac crest to be placed subperiosteally either through the alar base incision or more commonly through an incision into the buccal sulcus at the level of the canine as an onlay graft on the piriform rim; this corrects both deformities simultaneously. The lateral vestibular mucosal defect on the cleft side was closed in a V-Y fashion and the skin redraped. The alar base was repositioned by making crescent-shaped incisions at the alar base perpendicular to the alar crease. A wedge excision of the nasal floor and alar cinch on the cleft side gives a good approximation of the alar base. The sills of the nostril were constructed by vertically mismatching the margins at the time of closure: the staggered margins were then turned in to create a ridge and heal by third intention. Although the nasal skeleton was repositioned well and looked symmetrical, an alar web was still noticeable alter the skin has been redraped. A small triangular medially-based skin flap was therefore raised from the web, trimmed, and transposed intranasally into the vestibule. This achieved a three-dimensional Z-plasty for reduction of the alar web.
Additional procedures such as revision of the lip and Scar, Le Fort I osteotomy, and an Abbe flap were also done in some cases. A plaster of paris splint (2) was applied for four weeks to maintain the corrected contour of the nostril, and to fix the healing nasal bones, and a “Koken-like splint" (4) was given to stop the nostril constricting again. Postoperative maintenance of the airway, and prophylactic care of the eyes is essential.
RESULTS
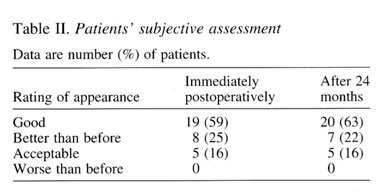
The immediate postoperative period was uneventful in all cases. After two years follow up, the aural cartilage graft had shrunk in two of four patients. The shape memory of the lateral alar cartilage resulted in mild relapse in seven cases. No sensory loss was reported. No slipping of the graft reported as happens in alloplastic implants. Patients’ subjective assessment of their postoperative appearance is shown in Table II.
None of the patients rated their appearance worse than before. None of the cases needed revision. There were no hypertrophic scars, no signs of nasal obstruction, and no exposure of hairy nares. The main advantage of this technique was the creation of a symmetrical and well-projected nasal tip.
DISCUSSION
It is universally agreed that repair of the nose deformity associated with a cleft lip is a formidable challenge that needs exact analysis, careful planning, and an atraumatic operative technique that is possible only through open direct visualisation through a transcolumellar incision (4, 12, 13). Only the open technique can provide the visual field essential for the accuracy of the correction. The primary advantage of the open approach is in the precise diagnosis of the deformity and the potential to repair displaced and deformed cartilage in an anatomical fashion. Wide exposure also makes mobilisation of the alar cartilages easy. Cronin and Denkler (4) used a “flying bird” or transcolumellar incision, because the vestibular lining of the lateral crus should remain attached to preserve vascularity and give support.
Several techniques including non-surgical methods (1) have been tried to achieve symmetry, but the management of the cleft lip and palate usually includes multiple primary and secondary operations to correct the deformity. We have described a one-stage method for the secondary management of the nose, which minimises both discomfort and cost to the patient. Although several authors have recommended primary rhinoplasty (15, 16, 21, 22), but as reported by Wray (26), about 30% of patients will require a second operation for correction of the nasal abnormalities even after a primary correction. Salyer (21, 22) wrote that 20% of his 400 patients who had had primary rhinoplasty required a secondary rhinoplasty to achieve the desired symmetry. He concluded that secondary corrective procedures focus mostly on skeletal support and distortions of the lining as well as on the rearrangement of the lower lateral cartilages. At the final stage, the aesthetic appearance can be improved by remodelling the contours with the addition of cartilaginous or bony implants. Takato et al. (24) in 1995 reported undesirable features in early correction of unilateral cleft lips. They attributed the reason to the use of an open surgical technique, and early mobilisation and suspension of the alar cartilages. McComb (12) and McComb and Coghlan (13) after a longitudinal review of their primary rhinoplasties reported residual asymmetry of the nostrils caused by septal deviation persists into adulthood and warrants secondary correction. Mulliken and Martinez-Perez (16) in 1999 reported that 80% of patients needed or will need a secondary rhinoplasty after primary repair of the unilateral cleft lip and nose using Millard’s rotation advancement technique. It is agreed that the nose with a severe deformity is difficult to correct by primary rhinoplasty alone because of the underlying skeletal deformities and it requires secondary rhinoplasty (4, 5).
Pigott (20) in 1985 highlighted the importance of securing the upper lateral cartilage to the septum, and the medial and lateral crus of the lower lateral cartilage to the upper lateral cartilage.
Ortiz-Monasterio and Ruas (17) in 1989 specified that besides repositioning the lower lateral cartilage, lengthening the columella and bringing it to midline, and correcting the asymmetries of the nasal floor, additional structural support in the form of bone and cartilage grafts are required to achieve adequate projection and angularity. Sheen (23) described a graft procedure by which a heart-shaped conchal or septal cartilage was fixed to both the domes with non-absorbable sutures to obtain both projection and increased angulation at the columellar—lobar junction.
Peck et al. (19) used an “umbrella graft” that consisted of a vertical cartilaginous strut between the medial crura and a horizontal onlay graft that overlay the alar dome. Umbrella grafts support the nasal tip pyramid and re-establish the projection of the nasal tip. Takato et al. (24) in 1995 advocated the use of a strut graft to contour the columella and define the tip. The correction of the tip by anterior reinsertion of a septal chondral graft through open exposure of the nasal frame has been emphasised.
Long-term stability of raised and repositioned cartilages is improved by direct suturing together by Skoog’s mattress key stitch as reported by Ozcan (18). Superior correction is possible in case of severe, septal, bony, nasal deformities. The scar is concealed by the modified transcolumellar incision at the root of the columella. V-Y plasty of the nasal mucosa on the cleft side gives exceptional correction of the alar webbing (2). Lengthening of the columella provides structural support for the columella and reduces the tension on the redraped nasal skin (4). Correction of the soft tissue along with the bony and cartilaginous deformities gives a good contour to the nose. This relatively simple, one stage procedure is ideal for creating the optimal nose in patients with unilateral CLP.



